- HOME
- LATEST
- ABOUT GPC
- NEW HERE?
-
MINISTRIES
- Ministry Awareness: Opportunities to Serve
- Care Group
- Church Wide Bible Study (CWBS)
- Family Ministry
- Filipina Fellowship
- Indonesian Fellowship
- Mission Ministry
- Music Ministry
- Outreach Ministry
- Precept Bible Study Ministry
- School Ministry
- Senior Adults Fellowship (SAFE)
- Sunday School
- Women Ministry
- Youth and Young Adults Ministry
- RESOURCES
- CONTACT US
- GIVE
- 中文部
My family in Christ, thank you for holding our family in prayer during this tender season. I want to share honestly with you—not as a pastor who has answers neatly arranged, but as a fellow pilgrim learning, once again, what it means to trust God together.
Life, I am learning afresh, is a series of tough decisions. And few decisions are as weighty as those we face near the end of life.
Three weeks ago, my mother-in-law fell at home and broke her hip. She was sent to the hospital immediately. At 90 years old, the question of surgery was not straightforward. Operating carried real risks, especially to her heart. But not operating meant she would likely be bedridden for the rest of her life, with its own cascade of complications and suffering.
After careful assessments, the doctors decided to insert four coronary stents to stabilize her heart. Under normal circumstances, she would need about a month of rest before any major surgery. But a month of immobility at her age would also cause serious physical decline. After
many discussions, and after being fully informed of all
the risks, my mother-in-law made her decision quickly and clearly. She agreed to proceed.
She told us she was not afraid.
More than that, she said she longed to be with the Lord.
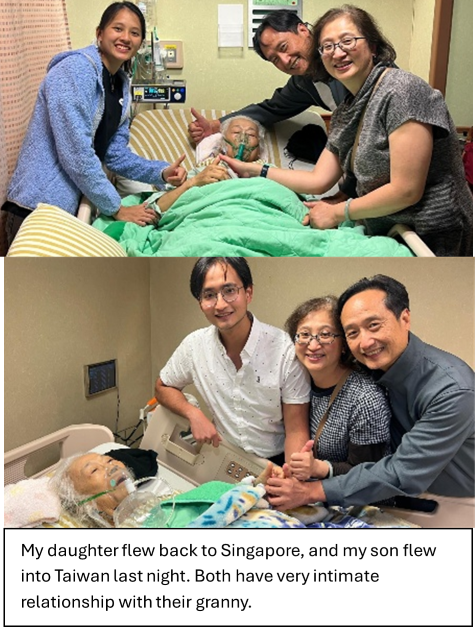
Her hip surgery was done just three days after the stent insertion, and medically, it went very well. But a few days later, her condition worsened. Her heart grew weaker. Her kidneys began to fail. Last Friday, her breathing became difficult and she drifted in and out of consciousness. When my wife messaged me about a sudden drop in her heart rate, my daughter and I booked the earliest flight and flew to Kaohsiung overnight.
I prayed a very simple prayer: “Lord, please let me see her alive.”
God answered that prayer. When I arrived, she was still awake and conscious.
That same day, I witnessed one of the most sacred and painful moments of this journey. My mother-in-law signed an advance directive indicating no intrusive life-sustaining treatment—no intubation, no cardiopulmonary resuscitation, no emergency measures to prolong life artificially. In medical terms, this is often referred to as DNR/DNI (Do Not Resuscitate / Do Not Intubate). What she wanted was clear: she wished to go peacefully, without invasive interventions.
That evening, as a family, we gathered around her bed. We prayed. We sang. We worshipped. We celebrated Holy Communion together. It reminded us of my late father-in-law’s final days—he had made the same request before he went home to the Lord. We wanted her to see, one more time, the whole family gathered at the Lord’s Table.
After Communion, my brother-in-law—also a pastor—anointed her with oil, from head to heart, from hands to feet. The fragrance of oil lingered in the room, a quiet reminder that she belongs to Christ, wholly and finally.
That was Saturday evening. We told her we would return the next day to worship with her again.
Early Sunday morning, around 4am, my brother-in-law received a call from the hospital. Her breathing had worsened. The staff wanted to reconfirm that the family understood her decision—no invasive treatment, not even electrical resuscitation if her heart were to stop.
When we arrived, she was still conscious. So we held church, right there at her bedside.
I led worship. My brother-in-law shared a short exhortation. Then I invited each family member to share how my mother-in-law had shaped their lives and their faith. The room was filled with gratitude, tears, laughter, and love. It was holy ground.
She listened. She knew what was happening. She responded when she could. And yet, she was struggling.
She could not sleep. She felt cold and was covered with layers of blankets, yet she perspired heavily. Because of her hip surgery, she could not turn easily. Her heart was failing. Oxygen was given to ease her breathing. Her kidneys were failing too—and a new question emerged: Should dialysis be started?
My son flew in last night when her heart rate dropped again. As we learned more, he shared a hard truth: without dialysis, toxins would build up, and she might eventually die from fluid overload—essentially “drowning” from within.
So how do we decide?
What counts as intrusive treatment, and what counts as comfort care? How do we relieve suffering without violating her clearly stated wishes? How do we honour her dignity while watching someone we love struggle?
Here is one of the hardest tensions I have ever felt: Doctors are trained—and rightly so— to make patients better, to intervene, to prolong life. But in this moment, the family’s calling is different. We are not trying to extend life at all costs. We are trying to help her go comfortably, gently, and peacefully.
We are walking together as a family, but we do not know what the next step will be.
Only God does.
And so we wait. We pray. We trust.
Some days, trust feels strong. Other days, it feels fragile and trembling. The waiting is heavy. The decisions are exhausting. The grief begins even before the goodbye.
Yet even here, God is present.
My family in Christ, I share this not to burden you, but to invite you to walk with us—and to grow together.
This journey has reminded me that discipleship is not only about serving, planning, or doing. Sometimes, it is simply about staying—staying with the dying, staying with the grieving, staying with God when answers are unclear.
Thank you for praying. Thank you for loving us. Thank you for being the body of Christ to our family.
Please continue to pray—not only for my mother-in-law’s peace and comfort, but also for wisdom, courage, and gentleness for all of us who must make these decisions with love.
We wait. We trust. And we hold on to the hope that whether in life or in death, we belong to the Lord.
Building His Missional Community,
Ps Forest
19 Jan 2026
